ARTICLE
Normamed, August 1st, 2024
Publications for Cause Medicine
August 2024 doi: 10.61029/normamed.2024.04.en
DOWNLOAD ARTICLEKeywords
For the diagnosis and therapy of sleep disorders.
Karl Tesmer, Robert Krokowski (Normamed)
Abstract
Infections, digestive disorders and organ dysfunction are often underlying causes of sleep disorders and non-restorative sleep. This is the result of the evaluation of two diagnostic observation studies and a subsequent treatment monitoring of 166 patients with chronic sleep disorders.
The patients were examined in parallel using general medicine, laboratory medicine and microbiology as well as the diagnostics of traditional Chinese medicine. Digestive disorders were found in 92 percent of the patients, organ dysfunctions in 70 percent and infections and mixed infections in 79 percent.
The patients were then treated for these infections and organ dysfunctions. The monitoring of treatment outcomes underlines that these are often root causes of sleep disorders. It also shows that after the treatment of the physical causes, patients sleep more peacefully in the long term, despite stress and psychological factors.
Digestive and organ disorders are often correlated with chronic sleep disorders. These can therefore also be the result of a chain of causes in which an infection-related spleen overload leads to a kidney overload (spleen-kidney yin weakness) and interacts with other organ dysfunctions (liver and heart). For many doctors and patients, such correlations have never been seen before.
An open-minded approach to therapy and continuous compliance on the part of the patients are prerequisites for successful treatment through integrated causal medicine (simultaneous coordinated diagnostics and therapy using both modern western medicine and traditional Chinese medicine). In 90 patients with high compliance, the treatment produced improvements in sleep that ranged from good to very good in 87 per cent; whereas in 23 patients with low compliance, only 35 per cent reported improvements that ranged from good to very good.
The treatment monitor also shows that patient compliance is strongly dependent on financial conditions. A change in thinking on the part of service providers and recognition of the results of causal treatment could be a social contribution to reducing costs in the healthcare system. If payers were to cover services of integrated cause medicine, then long histories of suffering from chronic diseases would be avoidable in many cases.
Treatment monitoring also reveals that patient compliance is heavily dependent on financial framework conditions. A change in the way healthcare providers think and the recognition of the results of causal treatment can contribute to reducing costs in the healthcare system. If the healthcare providers were to take over the services of integrated causal medicine, then long histories of suffering from chronic diseases would be avoidable in many cases.
1Introduction
Sleep disorders/non-restorative sleep (insomnia) are medically defined as symptoms that persist for more than six months and permanently impair people’s quality of life and performance. Chronic sleep disorders are divided into “acute” (up to about four weeks) and “subacute” (which develop insidiously and over a period of six months). (1)
Untreated infections, especially with pathogenic yeasts of the Candida species and with bacteria such as Helicobacter pylori, and also parasites can be part of the causal chain of sleep disorders if undetected or untreated. This is because such infections cause an overload of the immune system and permanently damage the spleen. This in turn can lead to kidney dysfunction and impaired liver performance. Organ dysfunctions and infections in interaction often become visible through digestive disorders. If these processes remain causally untreated and only their symptoms are treated (for example, with painkillers, sedatives or digestive aids), then complaints can become chronic. In addition to psychological effects (including depression), these also include sleep disorders/non-restorative sleep patterns in particular.
Chronic sleep disorders can indicate that the above-mentioned interactions have been working as physical processes for a long time. In these processes, non-restorative sleep then affects the performance of the organs. This favours immune deficiencies and susceptibility to renewed or further infections.
The result is a cycle of causes and interactions that can often only be recognised through comprehensive diagnostics and treated with integrative medical measures.
These experiences from medical practice were the guiding principles for two diagnostic observation studies and a treatment monitoring. Against their background, the same context was examined from three perspectives. The aim of the observations was to verify the medical experience that the treatment of infections and organ dysfunctions in the restoration of well-being and performance also showed a clear improvement in sleep quality.
Diagnostics by general medicine, immunology and microbiological laboratory medicine were carried out at the MVZ Ärztehaus Mitte in Berlin by the specialist in immunology and laboratory medicine Dr. Sebastian Pfeiffer. (2)
Complementary medicine diagnostics were carried out in the traditional Chinese medicine practice of Wang/Xie in Berlin, under the direction of Bei Wang, senior physician (Shanghai) and non-medical practitioner. (3)
The coordination of the treatments as well as the monitoring of the treatment successes in the MVZ and in the TCM practice was carried out by Stefanie Kopf, Study Nurse in the MVZ Ärztehaus Mitte, and colleagues. (4)
This was also done in cooperation with the pharmacist Sabine Olivar, “Apotheke im Regierungsviertel” Berlin, who was available as a supportive advisor to the patients for the individual adaptation of TCM herbal formulations.
The duration of the studies was four years, including a preparation period of almost eight years. This was due especially to the establishment of the combination between modern western medicine, microbiological laboratory medicine and traditional Chinese medicine. It was also necessary to introduce study-specific coordination and quality assurance routines for the complex patient management based on Normamed standards. This served both to ensure the quality of the examination results (e.g. through special guidelines for microbiological sample collection) and to ensure the highest possible patient compliance. In this respect, the “pilot task” assigned to the Normamed service in the medical centre and in the TCM practice proved to be an important component for successful treatment.
Infections and organ dysfunction tend not to be the focus of scientific interest in studies on sleep disorders. Although it is recommended to focus on the effects of infections on chronic symptoms, the number of studies on this topic is rather low compared to other approaches (e.g. sleep apnoea, psychosocial reasons, psychological stress). Thus, even a recommendation by the Robert Koch Institute in 2004 on the pathogenetic significance of intestinal Candida colonisation (5) has since hardly led to any studies investigating the aforementioned connection. “As always, when the data availability is unsatisfactory, there is room for speculation. Such an unsatisfactory situation for patients as well as for the treating physicians can only be defused by diligent studies and the associated growth in knowledge.” (5: 596) This recommendation of the RKI has so far remained unconsidered with regard to the correlation of sleep disorders and infections and organ dysfunctions.
The reasons for the reluctance of scientists to address the aforementioned causal cycles and interactions in studies are certainly also to be traced back to a scientific medical culture that makes studies on complex interrelationships very difficult. Especially when people suffer chronically, when their quality of life is greatly impaired by physical symptoms, even pain and despair, they need medical treatment. Conducting studies with such people over longer periods of time, which are randomised and conducted in a double-blind format, involving control groups and even placebos, and thus meeting the requirements of so-called evidence-based medicine, is profoundly contrary to medical ethics, which cannot approve of such human experimentation.
The plausibility of causal chains and treatment options can therefore only be gained if patients allow themselves to be observed voluntarily during their examinations and the treatments that subsequently ensue. This presupposes a high degree of willingness to cooperate on their part. The pressure of suffering in the case of chronic sleep disorders certainly promotes compliance at first. For sustainable treatment success, however, the patients’ compliance must be achieved over a long period of time. In the case of treatments that are carried out by both conventional and complementary medicine, there are also interdisciplinary requirements for the treatment combination. Long planning is necessary as well as the assurance of the implementation over a longer period of time. For this, the patients need care that goes beyond the usual level of studies and treatment monitoring. Additional complications include fears of medical routines, such as those imposed during the Corona pandemic. For doctors, too, the combination of different medical perspectives is a major challenge. Medicine has always been a process of change, in which new findings led to changes in the direction of diagnostics and therapy. And such change has never progressed without resistance, even if it ultimately served the well-being of patients.
With the two diagnostic observation studies and the treatment monitoring, comprehensive results of long-term observations on the causation of sleep disorders by infections and organ dysfunctions are now available for the first time, conducted over a period of four years from 2018 to 2022. These results highlight the need to further investigate causal medical and scientific correlations. Therefore, the long-term observations of the aforementioned studies will also be continued and extended to other symptoms (from 2023: migraine/headaches).
2Causal medical diagnosis and treatment of sleep disorders
According to the results of the 2015 Study on the Health of Adults in Germany (DEGS1), 30.3 percent of women and men suffer from problems falling asleep or sleeping without interruption (three times a week or more). (6) In modern Western medicine, sleep disorders are considered in the context of an “insomnia syndrome”. If women and men suffer from interruptions falling asleep three or more times a week, have reduced sleep quality and report daytime sleepiness and/or fatigue, they are considered “positive” in this respect. For “insomnia syndrome”, the prevalence was 7.7 percent for women and 3.8 percent for men. For those with low social status, women had a higher risk for the presence of insomnia syndrome than men. According to DEGS1, stress, depressive symptoms, burn-out syndrome and sleep disorders are closely related. With increasing stress levels, it is said, the burden of depressive symptoms, burn-out syndrome and sleep disorders also tends to increase. According to the survey, only 17.0 percent of people with below-average stress levels suffer from at least one of these three disorders, whereas 61.1 percent of people with high stress levels are afflicted. It should be noted that, on the one hand, a high stress level promotes the development of other disorders, but it is also possible that, for example, sleep or anxiety disorders increase the subjective experience of stress. (7), (8)
The results of the diagnostic observation studies and the treatment monitoring on the connection between sleep disorders, infections and organ dysfunctions, which are considered in the present analysis, point to connections that are hidden in such statistics. The results suggest that sleep disorders should not only be considered in connection with psychosocial factors, but also as a result of physical processes in the context of an epidemiological event that often goes unnoticed. For example, infections with pathogenic yeasts of the Candida species and infections with bacteria such as Helicobacter pylori are still “common diseases”. According to the results of the observational studies analysed in the following, their neglect seems as negligent as the general focus of today’s medicine on the consequences of viral infections and a relatively high neglect of microbiology. While a plethora of clinical studies speculate on the consequences of infections with new viruses for fatigue states, long-known causative agents of many symptoms are downplayed or ignored.
Causal chains and interactions in sleep disorders naturally include physical and psychological processes. However, chronic sleep disorders are often preceded by a creeping, often imperceptible process in which undetected or untreated infections lead to organ dysfunctions – especially of the spleen, kidneys, liver and gall bladder. Over time, these dysfunctions become noticeable in particular through digestive disorders such as diarrhoea, constipation and changing stool patterns, heartburn and intolerances, but also through other symptoms. These include joint disorders and pain in the limbs, frequent bladder infections, skin problems, exhaustion and burnout, as well as sleep disorders in particular.
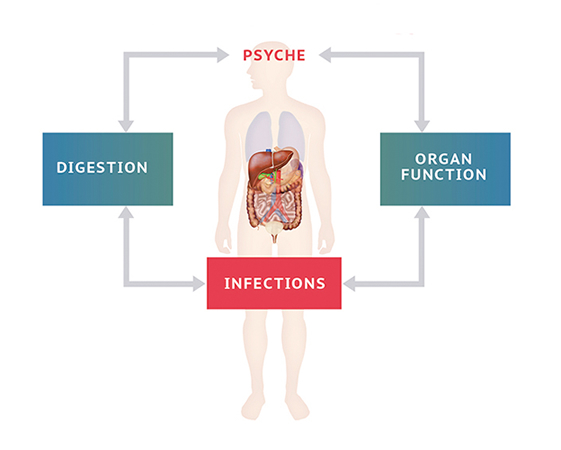
If such disorders tend to stabilise, they can in turn have an effect on digestion and organ activity, interact with other disorders and, for example, have an effect on the immune system via the dysfunction of the spleen, so that the body’s protection against the effects of new infections progressively decreases to a greater extent. In the case of chronic symptoms, a cycle of effects has often developed that is difficult to break down causally and often requires comprehensive medical knowledge and a great deal of experience (Fig. 1). In many cases, this results in the abandonment of causal medicine and the treatment of individual symptoms.
Fig. 1 Infections, Digestive Disorders And Organ Dysfunctions Influence Mental Processes And They Interplay With Bodily Processes
A key organ in the process of interaction is the spleen. It has an important regulatory function between the immune system and organs, especially in the case of infections – and its condition reflects the level of stress in the body. Infections cause an overload of the immune system and permanently damage the spleen. This in turn can lead to kidney dysfunction and impaired liver performance. Organ dysfunctions and infections in interplay often come to light through digestive disorders.
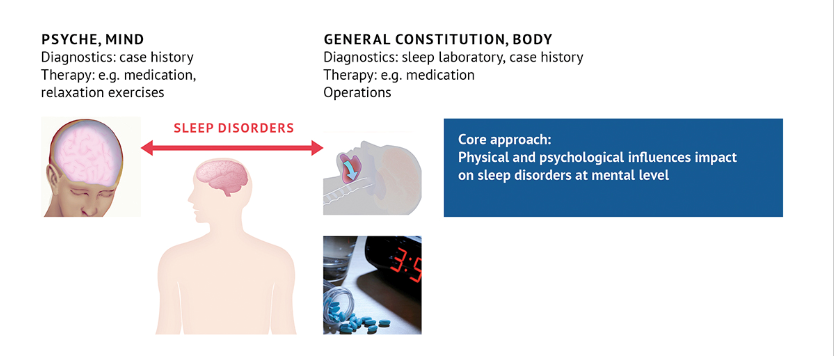
It is therefore astonishing that in modern western medicine such whole-body processes are rarely echoed in studies. There is a clear emphasis on psychological factors and on mechanical physical factors that can be investigated in sleep laboratories (cf. section 2). Accordingly, the diagnosis and treatment of sleep disorders also focus on these interrelationships (Fig. 3). In modern western medicine, sleeping pills are still the first choice for the treatment of sleep disorders, along with stress reduction and exercise regime.
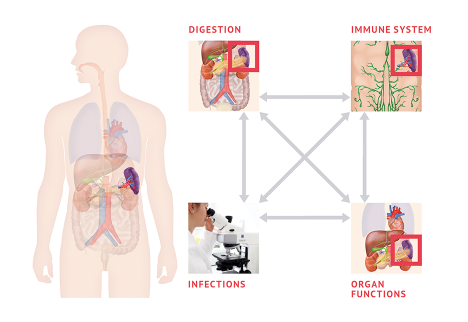
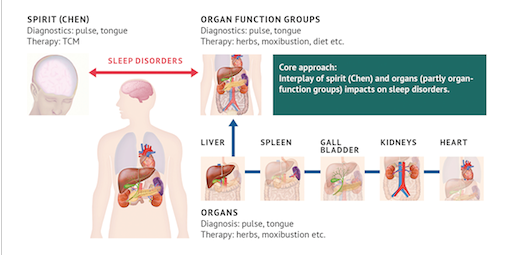
It is only possible to a limited extent to understand complex bodily processes in context and in their course by means of the diagnostic techniques of modern western medicine – it often lacks the opportunity for observation of small changes. As informative as laboratory values and imaging procedures are, they always provide only a snapshot of the physical condition. Traditional Chinese medicine has finer differentiation possibilities, especially when it comes to organ dysfunctions in interaction (Fig. 4). Here too, however, there is a neglect of infections in the chain of causes. In both modern Western and traditional Chinese medicine, the lack of systematic consideration of microbiology is one reason for the exaggerated evaluation of the psychological factor as a causative factor for sleep disorders.
It is only the combination of modern western medicine with traditional Chinese medicine and both with microbiology that facilitates a causal medical diagnosis and therapy for many symptoms that are the result of chains of causes and interactions (Fig. 5). At first it is helpful not to immediately put psychological factors in the foreground of the diagnosis. This can influence decisions on therapy in a one-sided way. However, this also generally shapes the medical assessment of sleep disorders, which can have problematic consequences not only for patients but also for the health care system.
3Sleep disorders in the view of modern western medicine
The usual diagnosis and therapy of sleep disorders within the framework of modern western medicine is confronted with permanently high numbers of people who chronically suffer from non-restorative sleep. Statistical observation shows that permanently ineffective treatments incur high costs in the health care system. Often, follow-up costs are not included, such as those caused by psychological problems that can also be caused by sleep disorders. Since the health insurance providers are primarily oriented towards the catalogue of measures of modern western medicine, the path of integrative treatment is blocked for many patients. The necessary compliance of the patients clashes with expensive private treatment costs. (9)
This connection can be seen, for example, in the federal health report, which is jointly supported by the Robert Koch Institute and Destatis. (10) In this, sleep disorders are assigned to the module “mental health” along with anxiety disorders, depressive disorders and alcohol dependence, among others, because they are considered factors that contribute to the development of mental disorders. (10: 114) As a result, the classification classifies sleep disorders as diseases of the nervous system or disorders of the psyche and behaviour:
“Insomnia is one of the most common sleep disorders. According to the ICD-10, the following criteria must be present for the diagnosis of (non-organic) insomnia: problems falling asleep or sleeping without interruption three times or more per week for a period of at least four weeks, as well as a poor quality of sleep. In addition, daytime sleepiness, fatigue or impairment of social functioning must be present as a result of the sleep problems. Depending on the presumed organic or psychogenic cause, insomnia is classified in the ICD-10 (International Classification of Diseases in the tenth revision) as G47 Sleep disorders (Chapter VI Diseases of the nervous system) or F51 Non-organic sleep disorders (Chapter V Mental and behavioural disorders).” (10: 116)
Sleep disorders are thus considered to be caused by psychological problems such as depression (11), as well as by behavioural problems such as lack of exercise, by occupational or family stress (12), (13) or by underlying diseases such as hypertension or diabetes (14):
“Sleep disorders are associated with a variety of physical and mental health disorders. For example, insomnia (…) is a risk factor contributing to the later onset of depression (…). Irrespective of age, insufficient sleep is related to becoming overweight and obese, hypertension as well as metabolic syndrome (a combination of the risk factors of obesity, hypertension, elevated blood lipids and insulin resistance) (…). In addition, sleep deprivation is associated with psychosocial impairments such as daytime sleepiness, poor concentration, stress, poorer general health and lack of psychological well-being (…).” (10)
Infections (especially Candida spec.) and mixed infections (especially Candida spec. and Helicobacter pylori) as well as organ dysfunctions caused by these have so far been little considered and studied in the aetiology of sleep disorders. (15)
In the S3 guideline “Non-restorative sleep/sleep disorders” of the German Society for Sleep Research and Sleep Medicine (DGSM) (16), infections are merely mentioned in general terms as a cause or contributory cause of sleep disorders, namely in connection with fatigue and states of exhaustion (16: 11), with viral infections of the CNS in lethal familial insomnia (16: 25), in hypersomnia (16: 38), especially in recurrent hypersomnia in Kleine-Levin syndrome (16: 92), in sleep apnoea in infancy as possible triggering factors (16: 136).
The S3 guideline (“Sleep/sleep disorders”) does not pay special attention to the possible connection between infections with pathogenic yeasts and sleep disorders. Pathogenic yeasts are not taken into account due to a lack of studies and only viruses, bacteria and parasites are considered. (17) Organ dysfunctions and their role in causing sleep disorders are also not systematically considered in the S3 guideline. Although organ dysfunctions are discussed in the context of differential diagnosis (e.g. enuresis nucturna) (16: 111), an interaction with infections and disorders is not considered, a connection with disorders of the immune system is only hinted at (16: 38), and an autoimmune basis is only suspected in the context of Kleine-Levin syndrome (16: 92).
Against this background, the observational study “On the possible connection between sleep disorders, infection-related gastrointestinal diseases and organ dysfunctions” (2) was dedicated to the aforementioned connection from the perspective of modern Western medicine. The study describes how “in order to motivate further studies as well as the consideration of infections in the therapy of subacute and chronic sleep disorders (insomnia) (18) (…) infections should be carefully documented by means of laboratory diagnostics and, as far as possible (…) organ dysfunctions should be recorded by means of laboratory analysis, sonography and ECG”. (2) (For the distinction between acute, subacute and chronic sleep disorders, see the discussion of the results of the procedure and the present study in section 6).
The observational study describes possible interactions between physical and psychological processes also from an immunological point of view and refers to studies that examine the interactions between brain activities and activities of the immune system in connection with infections.
In this context, infectious diseases are associated with sleep disorders. The studies reviewed show how Candida albicans and Helicobacter pylori can cause sleep disorders when they affect the respiratory (19) and endocrine (20: 13), (21) systems as well as the digestive (22: 11), (23) system.
So if pathogenic yeasts and bacteria are so linked to sleep disorders via interactions between physical and mental systems, then it is plausible to ask what impact infections and their primary organ dysfunctions (of the spleen, liver and kidneys) have on sleep. The observational study places its focus on the development of chronic sleep disorders as a result of cumulative and combined organ dysfunction arising from infection-related overload of the spleen and, subsequently, the kidneys. In this respect, the results of this study suggest a new approach to the question of the causation of sleep disorders even in modern Western medicine.
4On the relationship between sleep disorders, infectious gastrointestinal diseases, and organ dysfunction from the perspective of modern Western medicine.
In the observational study “On the possible association between sleep disorders, infection-related gastrointestinal diseases and organ dysfunction” (2), 166 patients of a medical care centre for integrative medicine were included in the observational studies from August 2018 to April 2022.
The duration of the patients’ sleep disorders at start of the study was between 1 and 5 years in 73 patients, between 6 and 10 years in 50 patients, and 43 patients reported having suffered from sleep disorders for more than 10 years. In this respect, all patients observed suffered from chronic sleep disorders.
According to the observational study, the patients were observed by evaluating serological and microbiological laboratory analyses, ultrasound examinations and the ECG. Serology, ultrasound and ECG were conducted using standard technical equipment. Special care was taken in microbiological material collection and evaluation as specified in the observational study. Sleep disorders of the patients were reported in the course of complaint treatment of the patients in the ongoing medical practice. A detailed medical history was taken to record the sleep disorders, which was documented in the observational study.
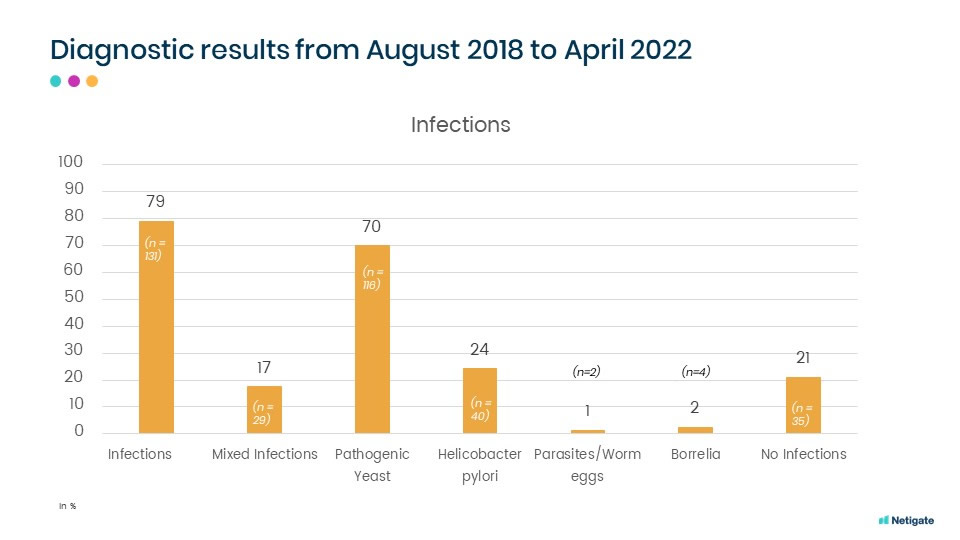
The results of the observational study showed that 92 percent of the 166 patients with chronic sleep disorders had digestive complaints, 79 percent had infections and 70 percent had organ dysfunction (cf. fig. 6). In 77 percent of the patients with sleep disorders, the pattern of digestive complaints ranged from striking to severe. The patients were also asked to rate their subjective perceived severity of symptoms in standardised anamneses using ten-point scales.
Infections with pathogenic yeasts were found in 70 percent of the patients in the observational study, infections with H. pylori in 24 percent and mixed infections in 17 percent (cf. Fig. 7).
The observations of the sonographic examinations revealed, in connection with sleep disorders, that 45 patients (27 percent) had apparent liver dysfunctions and 33 (20 percent) kidney dysfunctions.
These figures alone suggest a connection between organ dysfunction and sleep disorders in the presence of infections. However, the observational study points out that modern western medicine lacks a refined diagnostic technique to precisely determine the organ dysfunctions that may be relevant for sleep disorders. The use of ultrasound and serological laboratory analysis would yield an organ status and value picture that could be supplemented by, for example, the inclusion of pulse diagnostics of traditional Chinese medicine. Exactly this then became clear in the TCM diagnostic observation study carried out in parallel with the same patient collective (cf. section 6).
5Sleep disorders from the perspective of Traditional Chinese Medicine
In contrast to modern Western medicine, Traditional Chinese Medicine (TCM) has a rich history of experience that spans centuries. Sleep disorders are also discussed in the earliest written documents, for example in the Huangdi Neijing (24). The effects of spleen, kidney and liver disorders on sleep are discussed in connection with digestive disorders.
One difficulty in recognising the medical experiences and findings of TCM lies in the fact that these have been presented in the language of nature since the earliest times – and that modern Western medicine finds the absence of scientific terminology to be a “validity problem” regarding TCM.
Current developments in the field of diagnostics, in the mutual translation of scientific terminology and medical imagery, reveal that there are also abstractions in pictorial representations as in scientific terminology. The inclusion of TCM diagnostics in ICD catalogues (25) and the efforts of the WHO to promote standardisation of diagnostics through translation works (26) show that both Western and Eastern medicine can contribute broad insights into integrative medicine. (27)
However, in order to understand the value of TCM diagnostics from the perspective of modern Western medicine, it is still necessary to prove that both languages speak about the same facts. This is accomplished by the TCM study (3) presented below with reference to organ dysfunction in sleep disorders. However, it should be noted that modern Western medicine and TCM approach sleep disorders from different angles.
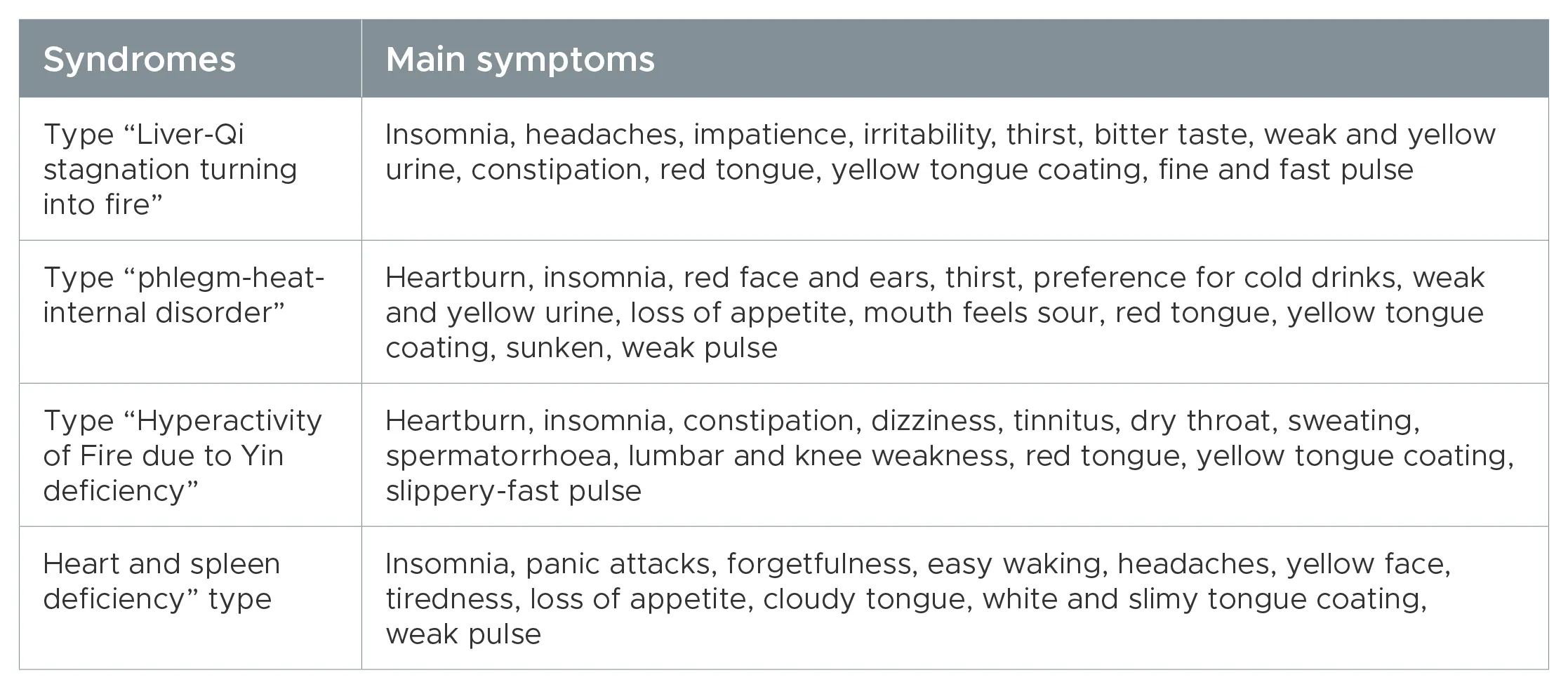
From a TCM perspective, the body is divided into five functional systems: Liver, Heart, Spleen, Lungs, Kidney, which are called “organ networks”. These networks control certain tissues, mental abilities and physical activities by regulating and maintaining the Qi (vital energy), blood and body fluids. In the collection of typical medical cases of Traditional Chinese Medicine, sleep disorders are classified under four syndromes. Main symptoms of these syndromes related to sleep disorders are closely linked to organ functions: the type “Liver-Qi stagnation turning into Fire” is controlled by the Liver, the type “Phlegm-Heat internal disorder” by the Lungs, the type “Hyperactivity of Fire due to Yin deficiency” by the Kidneys and the type “Heart and Spleen deficiency” by the Heart and Spleen (see Table 1).
Modern Western medicine is based on polysomnographic measurements (including electroencephalogram (EEG), electromyogram (EMG) and electrooculogram (EOG) signals). In device-based sleep monitoring, a distinction is made between wakefulness, REM phases (rapid eye movement, e.g. dreaming) and non-REM phases (e.g. deep sleep). (28), (29), (30) Other apparatus-based diagnostic methods, such as ultrasound diagnostics, are rarely used in sleep studies because of the suppression of organs such as kidney, liver and spleen dysfunction – and apparently only when TCM is in the context of the studies. (2)
In this respect, TCM and modern medicine have a totally different understanding of the classification of sleep. However, since the present analysis for the first time deals precisely with the inclusion of organ dysfunctions in the comprehensive aetiological consideration of sleep disorders, the understanding of TCM sleep disorder diagnostics is important both for the studies evaluated – and as a model for future studies on the value of integrative medicine. The examination of sleep through models of modern western medicine alone does not seem to make sense here – especially since there is no viable procedure analogous to non-apparative diagnostics of TCM in modern western medicine. When using TCM diagnostics systematically, it becomes clear that this is not the case. (3)
The often voiced criticism from the perspective of Western modern medicine of Traditional Chinese Medicine, that its diagnostic and therapeutic validity cannot be proven by quantitative measurement methods, often stems from ignorance of modern technological developments in TCM as well. This concerns both apparatus-based diagnostics (such as pulse and tongue diagnostics) and the use of intelligent diagnostic systems. Particularly promising here are combinations of artificial neural networks (KNN) (31) with expert systems (32) in the context of adaptive neuro-fuzzy inference systems (ANFIS) (33), (34), which integrate learning, association, recognition and information processing in the field of TCM and thus take account of the special features of complex organ networks. (35)
Within the diagnostic framework of TCM, each organ of the human body is considered an integral part of the whole. The organs work together, complement each other and interact well in a healthy state – and of course in the development of disease when disorders are present. The functional state of the internal organs can be mapped through the organs on the surface of the body (eyes, mouth, lips and tongue). When the function of the internal organs is damaged or diseased, the organs on the surface of the body will exhibit different signs. Traditional Chinese medicine determines the signals of damage through four diagnoses: examination by inspection, hearing and smelling, questioning and palpation.
During the inspection, the patient’s body shape, tongue, tongue coating and facial colour are examined. Based on changes, diseases can be localised and determined. Deviations from these in shape, coating, colour, moisture, etc. are indications of organ function disorders for the experienced TCM doctor. The appearance of the normal tongue is pale pink, slightly moist and shiny, often covered with a whitish-clear coating. If the spleen is disturbed, the tongue is swollen and a notch appears in the middle of the tongue. Changes in certain regions of the tongue can therefore indicate how organ functions are impaired (Fig. 9). The examination of the tongue can also reveal a suspected infection (to be tested microbiologically): A furrow or notch in the middle of the tongue indicates a stomach disorder, as is very often caused by an infection with Helicobacter pylori.
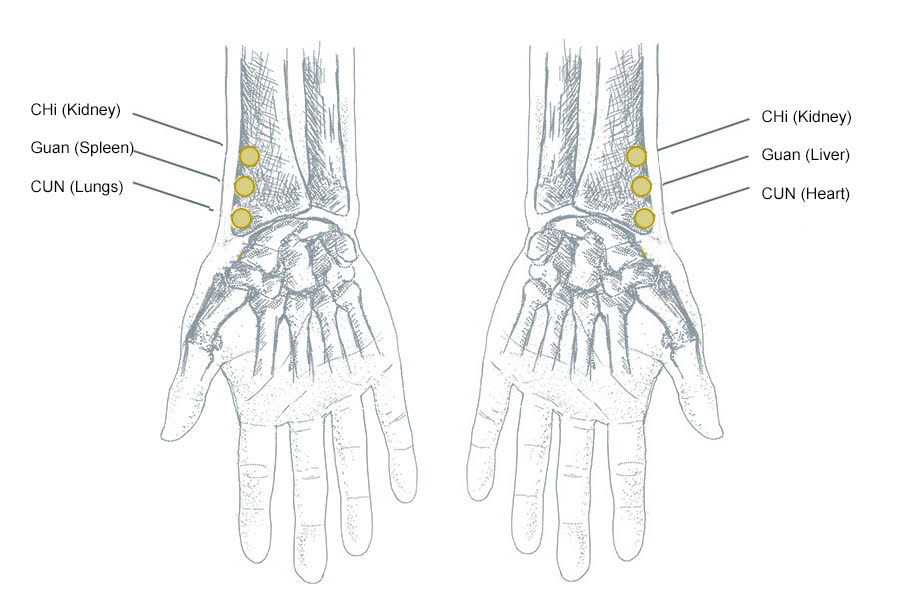
Accordingly, diseases are diagnosed by listening to the patient’s voice and assessing their body odour. The questioning takes the form of a thorough anamnesis and serves to check the systemic connections. This includes physical and mental sensations, personal and family history, previous medical history, time of onset and current symptoms. For example, various pulses of the patient are palpated, through which conclusions can be drawn about interactions of the organs in organ networks (Fig. 10).
The different pulse positions are each assigned to different organs: The type of pulse is determined at three levels (skin surface, middle and deep level). The volume, rhythm, frequency and form of the pulses are identified. This makes it possible to distinguish deficiency, fullness or disharmony in the organs and their functions. The pulse is palpated at three points on each wrist: From the hand (distal) towards the shoulder (proximal): Cun, Guan, Chi. Three levels of pressure are applied to each of these points by palpation: superficial, medium, deep. On the left wrist, the functional relationships are as follows: CUN – heart and small intestine, GUAN – liver and gall bladder and CHI – kidney and urinary bladder, kidney yin. On the right wrist, the functional relationships are as follows: CUN – Lung and Large Intestine, GUAN – Spleen and Stomach and CHI – Kidney and Ming Men, Kidney-Yang.
Experienced TCM doctors have many years of experience in practising pulse and tongue diagnostics and the traditional knowledge of both diagnostic areas. In the meantime, this has been incorporated into the development of corresponding diagnostic apparatus for pulse (36), (37), (38), (39) and tongue diagnosis (40), (41), (42), which will make a contribution to TCM diagnosis that is also “objectified” from the point of view of modern Western medicine through parameters and standards. (43)
The piece of wisdom “he who heals is right” is commonly shared non-publicly by doctors of modern Western medicine as well. At the same time, the validity of TCM is nevertheless frequently doubted by these same doctors. However, both the evaluation of observational studies (3), (2) and the monitoring of treatment successes (4) as well as the comparison between gastroenterological diagnostics and TCM diagnostics clearly show (44) that TCM already has a high value as a diagnostic instrument in integrative medicine, even without technical diagnostic apparatus. It is thus well established, that: The evidence base for standardising TCM patterns in ICD-11 can be improved if TCM diagnostic instruments are developed and rigorously validated within the framework of the COSMIN guidelines (COSMIN = Consensus-based Standards for the selection of health Measurement Instruments). These guidelines should be modified to take into account the characteristics and uniqueness of TCM diagnostic processes. (45) In this respect, the impetus of the correlations demonstrated in the studies should not only be used for the benefit of patients. The interaction of modern Western and Traditional Chinese Medicine can lead to reduced expenditure and lower costs in health care systems through increased efficiency.
6On the relationship between sleep disorders, infection-related gastrointestinal diseases, and organ dysfunction from the perspective of traditional Chinese medicine.
The study was conducted from August 2018 to April 2022 and enrolled 166 patients. All patients came from the patient collective of the MVZ Ärztehaus Mitte in Berlin and were also examined in the TCM practice at their own request in parallel to the diagnostics of the Ärztehaus. All patients suffered from chronic sleep disorders. In 79 percent of the patients, infections with pathogenic yeasts had been found by microbiological examinations of the medical centre and its special microbiological laboratory, in 24 percent infections with H. pylori and in 17 percent mixed infections (cf. above paragraph 4).
In addition to the observation of organ dysfunctions by laboratory analysis and sonography of the medical centre, the same patients were examined in the TCM practice by anamnesis, view, pulse diagnosis and tongue diagnosis. The observations of the TCM examinations revealed a high proportion of organ dysfunctions in correlation with sleep disorders (cf. Fig. 11), especially in the kidneys, liver and spleen. In addition to the organ dysfunctions determined by laboratory analysis and sonography, further organ dysfunctions were found, such that the quantity of patients with dysfunctions determined by specialist medicine (2) was a subset of the patients diagnosed with TCM.
Fig. 11 Frequency Of Organ Dysfunction Found In The Observed Patients Of The Study Using Sonographic And Laboratory Analysis, And Tcm Examinations.
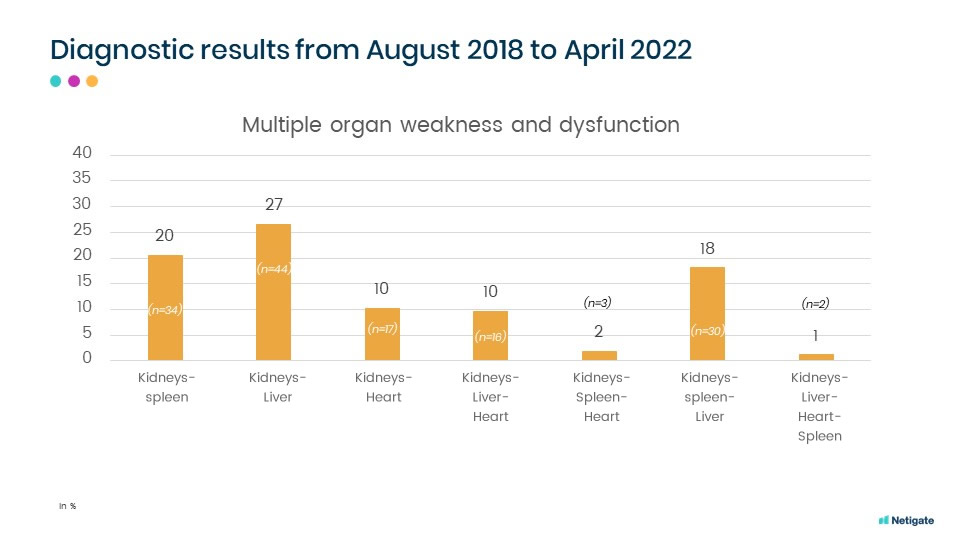
In the course of TCM diagnostics, multiple disorders were observed that occurred in combination (cf. Fig. 12).
Fig. 12 Frequency Of Combined Organ Dysfunction Found In The Observed Patients Of The Study Using Tcm Examinations.
The aim of the TCM diagnostic study was to observe the connection of patients with chronic sleep disorders (insomnia) with organ dysfunctions and the chain of causation of their development through TCM diagnostics. The study thus aimed to better understand the development and chronification of sleep disorders in the process of a progressive chain reaction.
Chronic sleep disorders in general stand on the tail end of a physical process. They are the result of a progressive chain reaction. In this process, an infection-related spleen overload can lead to a kidney overload (spleen-kidney yin weakness). This is combined with digestive disorders and other organ dysfunctions (liver and heart) in interactions. The purpose of the study was to examine the processes and their interactions with regard to the order in which they occur and to observe the connection between chronic sleep disorders and organ dysfunctions from the perspective of Traditional Chinese Medicine.
As expected, cumulative organ dysfunctions were observed in chronic sleep disorders, i.e. disorders of the kidneys (in 95 percent of patients), liver (in 58 percent), spleen (in 42 percent) and heart (23 percent). In combination, weakening was observed in kidney and liver (27 percent), kidney and spleen (20 percent), kidney and heart (ten percent); kidney, spleen and liver (18 percent), kidney, liver and heart (ten percent) and kidney, spleen and heart (two percent).
7The success of treating patients with chronic sleep disorders through combined therapy of modern Western medicine and Traditional Chinese Medicine.
From August 2018 to April 2022, two observational studies were conducted among patients at Ärztehaus Mitte in Berlin. (2), (3)
The treatment of the diagnosed clinical pictures (cf. above paragraphs 3 and 5) was carried out at the request of the patients by combining specialist and complementary medicine therapy. The efficiency review of the treatments within the framework of their monitoring and the evaluation of the collected data was also carried out at the request and with the consent of the patients. (4)
Following the specialist and complementary medical diagnosis, the sleep disorders were treated by causal treatment of the gastrointestinal disorders.
For the purpose of stabilising the metabolism and strengthening the organs, the treatment of the infections with antibiotics was supported by taking Chinese herbs and teas, as well as by individual nutritional counselling. Special TCM teas and herbs were used to treat physical processes, at the end of which, if left untreated, chronic sleep disorders also become apparent. The causal treatment included infection-related spleen overload and subsequently kidney overload (spleen-kidney yin weakness), as well as digestive disorders and other organ dysfunctions (liver and heart). Details on medication are deliberately omitted here, as on the one hand this was standardised and carried out according to guidelines, but on the other hand it was also supplemented or varied depending on the individual situation and individual findings. Nutrition and exercise recommendations were obligatory in this context, but also adapted according to intolerances or physique. Medications for underlying diseases (e.g. diabetes, blood coagulation disorders) were kept unchanged.
The patients were asked in standardised anamneses by means of ten-point scales about their subjective assessments of the severity of the complaints they perceived. They were asked to rate their sleep quality, their overall well-being and their digestion. Questionnaire-based online monitoring and telephone interviews were then conducted over a period of one year. The monitoring usually started one week after the start of treatment, the first three monitoring sessions at weekly intervals, then fortnightly, then monthly until the end of the sixth month. Before the final monitoring after one year, the patients were also called monthly between the sixth and twelfth month and asked about their well-being and living conditions by telephone on the basis of the questionnaire.
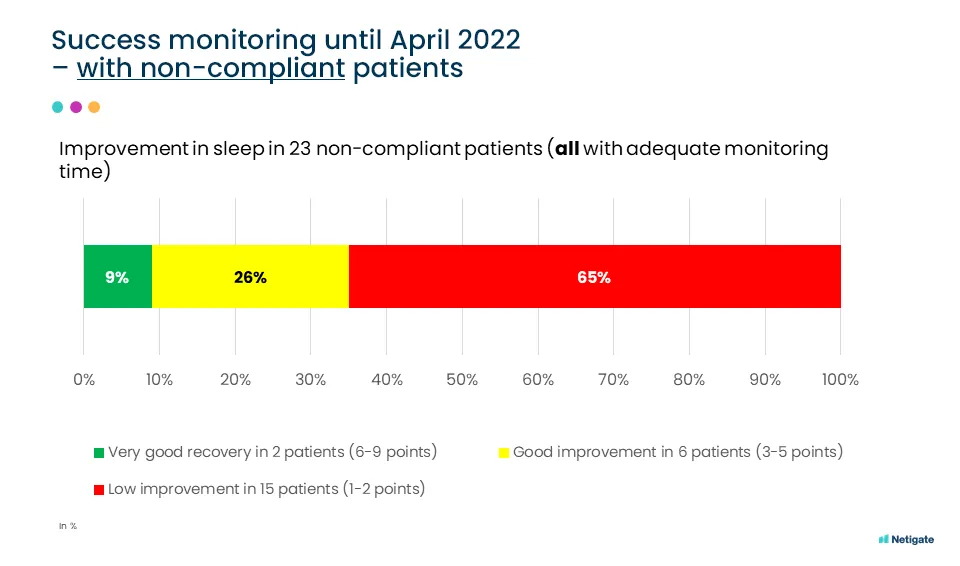
The monitoring showed that the success of treatment through integrated root cause medicine depended on the continuous compliance of the patients over a longer period of time. Accordingly, we observed that: In 90 patients with high compliance, the treatment showed improvement in sleep ranging from good to very good in 87 percent; whereas in 23 patients with low compliance, only 35 percent showed improvement ranging from good to very good (cf. Figs. 13 to 15).
The courses of improvement in individual patients clearly show the correlation in well-being between sleep disorders and compliance over a long period of time (6 to 12 months) (cf. e.g. Fig. 16).
It was also found that psychological factors, such as stress due to exceptional circumstances, could have a short-term influence on sleep patterns. However, with a simultaneous and stable improvement in digestion (reflecting organ health), a sustained improvement in sleep was often noted (Fig. 17).
8Summary
Infections, digestive disorders and organ dysfunctions are often the underlying causes of chronic sleep disorders and non-restorative sleep. This is the result of the evaluation of two diagnostic observation studies and a subsequent treatment monitoring of 166 patients with chronic sleep disorders.
The patients were examined in parallel using general medicine, laboratory medicine and microbiology as well as traditional Chinese medicine diagnostics. Digestive disorders were found in 92 percent of the patients, organ dysfunctions in 70 percent and infections and mixed infections in 79 percent.
The patients were then treated. The monitoring of treatment success underlines that infections and organ dysfunctions are often causative factors for sleep disorders. It also shows that after treatment of the physical causes, patients sleep more restfully in the long term, despite stress and psychological factors.
Digestive disorders and organ dysfunctions are often correlated with chronic sleep disorders. These can therefore also be the result of a chain of causes in which an infection-related spleen overload leads to a kidney overload (spleen-kidney yin weakness) and interacts with other organ dysfunctions (liver and heart).
Therapeutic open-mindedness and the continuous compliance of the patients are prerequisites for the success of treatment through integrated cause medicine (simultaneous coordinated diagnostics and therapy by both modern western medicine and traditional Chinese medicine). In 90 patients with high compliance, the treatment showed improvement in sleep ranging from good to very good in 87 percent; while 23 patients with low compliance showed improvement ranging from good to very good in only 35 percent.
The results of the diagnostic observation studies and the monitoring show that chronic sleep disorders of many patients can generally be averted if treated causally. Applied preventively, TCM measures can generally help avoid many sleep disorders or prevent chronicity even in the subacute stage. When the physical causes are treated, psychosocial factors and acute stress situations or pain remain triggers for sleep disorders, but these often remain short-term symptoms.
The high number of chronic sleep disorders in the majority of the population should be investigated against this background. After all, if general and sleep medicine measures focus, for example, on psychosocial symptom treatments (sleeping pills) or treatments for sleep apnoea, then there is a real threat that infections and organ dysfunctions will be overlooked as causes of sleep disorders/non-restorative sleep. Treatment monitoring also shows that compliance of patients is heavily dependent on financial framework conditions. A change in the way healthcare providers think and recognise the results of causal treatment could be a social contribution to reducing costs in the healthcare system. If the health insurance providers were to take over services of integrated causal medicine, then long histories of suffering from chronic diseases could be avoided in many cases.
Bibliography
-
Helbig, AK (2019): Zusammenhang zwischen Schlafstörungen und chronischen Erkrankungen: Ergebnisse bevölkerungsbasierter Studien, Dissertation Darmstadt 2019, p. 11–21, https://edoc.ub.uni-muenchen.de/23469/1/Helbig_Anna_Katharina.pdf accessed on March 7th, 2023.
-
Pfeiffer S (2024): Investigation of the relationship between sleep disorders, infection-related gastrointestinal diseases and organ dysfunction, Observational Study, Normamed. https://doi.org/10.61029/normamed.2024.01.en
-
Wang B (2024): Diagnostic observations of Traditional Chinese Medicine on organ dysfunction in patients with sleep disorders and infections, Observational Study, Normamed. https://doi.org/10.61029/normamed.2024.02.en
-
MVZ Ärztehaus Mitte Berlin (2024): Observational Study on the treatment of patients with chronic sleep disorders by combined therapy of modern western medicine and traditional Chinese medicine. The success of treatment to treat sleep disorders through infection eradication, organ function strengthening, nutritional counseling and digestive regulation, Normamed. https://doi.org/110.61029/normamed.2024.03.en
-
Robert Koch-Institut (2004): Pathogenetische Bedeutung der intestinalen Candidabesiedelung. Mitteilung der Kommission „Methoden und Qualitätssicherung in der Umweltmedizin“ Bundesgesundheitsbl – Gesundheitsforsch -, Gesundheitsschutz 2004 · 47:587–600. https://doi.org/10.1007/s00103-004-0860-1
-
Schlack R, Hapke U, Maske U (2013): Häufigkeit und Verteilung von Schlafproblemen und Insomnie in der deutschen Erwachsenenbevölkerung. Ergebnisse der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1). Bundesgesundheitsbl – Gesundheitsforsch – Gesundheitsschutz 56(5-6):740-748. https://doi.org/10.1007/s00103-013-1689-2.
-
Hapke U, Maske U, Scheidt-Nave C (2013): Chronischer Stress bei Erwachsenen in Deutschland. Ergebnisse der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1). Bundesgesundheitsbl – Gesundheitsforsch – Gesundheitsschutz 56(5/6):749- 754. https://doi.org/10.1007/s00103-013-1690-9
-
Maske UE, Riedel-Heller SG, Seiffert I (2014): Häufigkeit und psychiatrische Komorbiditäten von selbstberichtetem diagnostiziertem Burnout-Syndrom. Ergebnisse der bevölkerungsrepräsentativen »Studie zur Gesundheit Erwachsener in Deutschland« (DEGS1). Psychiat Prax (Epub) https://doi.org/10.1055/s-0035-1552702
-
Daley M, Morin CM, LeBlanc M (2009): The economic burden of insomnia: direct and indirect costs for individuals with insomnia syndrome, insomnia symptoms, and good sleepers. Sleep 32(1):55-64. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2625324/pdf/aasm.32.1.55.pdf accessed on March 7th, 2023
-
Robert Koch-Institut (Ed) (2015): Gesundheit in Deutschland. Gesundheitsberichterstattung des Bundes. Gemeinsam getragen von RKI und Destatis. RKI, Berlin 2015. https://www.rki.de/DE/Content/Gesundheitsmonitoring/Gesundheitsberichterstattung/GesInDtld/gesundheit_in_deutschland_2015.pdf?__blob=publicationFile accessed on March 7th, 2023.
-
Baglioni C, Battagliese G, Feige B (2011): Insomnia as a predictor of depression: A meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord 135(1-3):10-19. https://doi.org/10.1016/j.jad.2011.01.011
-
Furihata R, Uchiyama M, Takahashi S (2012): The association between sleep problems and perceived health status: a Japanese nationwide general population survey. Sleep Med 13(7):831-837. https://doi.org/10.1016/j.sleep.2012.03.011
-
Ohayon MM, Zulley J (2001): Correlates of global sleep dissatisfaction in the German population. Sleep 24(7):780-787. https://pubmed.ncbi.nlm.nih.gov/11683481/ accessed on March 7th, 2023.
-
Budhiraja R, Roth T, Hudgel DW (2011): Prevalence and polysomnographic correlates of insomnia comorbid with medical disorders. Sleep 34(7):859-867. https://doi.org/10.5665%2FSLEEP.1114
-
Riemann D, Baglioni C, Bassetti C, Bjorvatn B, Groselj LD, Ellis JG, Espie CA, Garcia-Borreguero D, Gjerstad M, Gonçalves M, Hertenstein E, Jansson-Fröjmark M, Jennum PJ, Leger D, Nissen C, Parrino L, Paunio T, Pevernagie D, Verbraecken J, Weeß HG, Wichniak A, Zavalko I, Arnardottir ES, Deleanu OC, Strazisar B, Zoetmulder M, Spiegelhalder K (2017): European guideline for the diagnosis and treatment of insomnia, Practice Guideline J Sleep Res, 26(6):675-700. https://doi.org/10.1111/jsr.12594
-
Deutsche Gesellschaft für Schlafforschung und Schlafmedizin (DGSM) (2009): S3-Leitlinie Nicht erholsamer Schlaf/Schlafstörungen, Somnologie 2009, 13:4–160. https://doi.org/10.1007/s11818-009-0430-8
-
Ibarra-Coronado EG, Pantaleón-Martínez AM, Velazquéz-Moctezuma J, Prospéro-García O, Méndez-Díaz M, Pérez-Tapia M, Pavón L, Morales-Montor J (2015): The Bidirectional Relationship between Sleep and Immunity against Infections, Journal of Immunology Research, Volume 2015, Article ID 678164. http://dx.doi.org/10.1155/2015/678164
-
Bericht des Robert-Koch-Institutes, Gesundheitsberichterstattung des Bundes, Heft 27, Berlin Oktober 2005, Schlafstörungen. http://www.dgsm.de/downloads/fachinformationen/rki-bericht/schlafstoerung.pdf accessed on March 7th, 2023.
-
Eichler L (2021): Retrospektive Analyse zur Untersuchung der Bedeutung von Polymorphismen in Chitinasegenen bei der CF-Lungenerkrankung, Dissertation Universität Tübingen. https://hsbiblio.uni-tuebingen.de/xmlui/bitstream/handle/10900/117684/Diss_Laura_Eichler.pdf?sequence=1, accessed on March 7th, 2023.
-
Kuschnereit M (2020): Demographie und Klinik des Polyglandulären Autoimmunsyndroms, Dissertation Mainz, 2020, p. 13. https://openscience.ub.uni-mainz.de/bitstream/20.500.12030/5443/1/kuschnereit_marie-demographie_un-20201202130458788.pdf, accessed on March 7th, 2023.
-
Perheentupa J (2006): Autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy. The Journal of clinical endocrinology and metabolism 91(8): 2843-50, https://doi.org/10.1210/jc.2005-2611
-
Tesmer K, Grünert B (1991): Gastritis mit Helicobacter pylori und Candida albicans. In: Pilzdialog, Praktische Mykologie, Jahrgang 1991, Heft 1, Schriftleitung: Prof. Dr. med. Dr. h. c. H. Rieth, Schwarzeck-Verlag, München, p. 11. https://www.normamed.com/pdfs/der-besondere-fallgastritis-mit-helicobacter-pylori-und-candida-albicans/ accessed on March 7th, 2023.
-
Treiber G, Kist M, Klotz U, Peitz U, Malfertheiner P (2005): Therapie der Helicobacter-pylori¬-lnfektion. Klinische, mikrobiologische und pharmakologische Aspekte. In: Deutsches Ärtzeblatt, Jg. 102, Heft 26, 1. Juli 2005. pp. A1883–1888, https://www.normamed.com/pdfs/therapie-der-helicobacter-pylori-lnfektion-klinische-mikrobiologische-und-pharmakologische-aspekte/ accessed on March 7th, 2023.
-
Veith I (1949): Huang Ti Nei Ching Su Wen, The Yellow Emperor’s Classic of Internal Medicine, Baltimore. https://archive.org/details/in.ernet.dli.2015.115032/page/n3/mode/2up , p. n224, n225, n262, accessed on March 7th, 2023.
-
Reddy B, Fan AY (2021): Incorporation of complementary and traditional medicine in ICD-11. BMC Med Inform Decis Mak 21 (Suppl 6), 381. https://doi.org/10.1186/s12911-022-01913-7
-
World Health Organization (2022): WHO international standard terminologies on traditional Chinese medicine. Geneva. Licence: CC BY-NC-SA 3.0 IGO. https://apps.who.int/iris/bitstream/handle/10665/352306/9789240042322-eng.pdf accessed on March 7th, 2023.
-
Man-Ki Poon M, Chung KF, Yeung WF, Hon-Kin Yau V, Zhang SP (2012): Classification of Insomnia Using the Traditional Chinese Medicine System: A Systematic Review, Hindawi Publishing Corporation, Evidence-Based Complementary and Alternative Medicine, Volume 2012, Article ID 735078, 9 pages. https://doi.org/10.1155/2012/735078
-
Andreotti F, Phan H, Cooray N, Lo C, Hu MTM, De Vos M (2018): Multichannel Sleep Stage Classification and Transfer Learning using Convolutional Neural Networks, 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Honolulu, HI, USA, 2018, pp. 171-174. https://doi.org/10.1109/EMBC.2018.8512214
-
Patanaik A, Ong JL, Gooley JJ, Ancoli-Israel S, Chee MW (2018): An end-to-end framework for real-time automatic sleep stage classification. Sleep, 41(5). https://doi.org/10.1093%2Fsleep%2Fzsy041
-
Boe AJ, Koch LLM, O’Brien MK, Shawen N, Rogers JA, Lieber RL, Jayaraman A (2019): Automating sleep stage classification using wireless, wearable sensors NPJ Digital Med., 2 (1), pp. 1-9. https://doi.org/10.1038%2Fs41746-019-0210-1
-
Tang AC, Chung JW, Wong TK (2012): Digitalizing traditional chinese medicine pulse diagnosis with artificial neural network. Telemed J E Health. 2012 Jul-Aug;18(6):446-53. https://doi.org/10.1089/tmj.2011.0204
-
Jiancheng H, Xiaoqian L, Fang H, Hongjuan H, Xuebin C, Yuanhui H (2013): Development of the Cardiac failure expert system for Chinese medicine diagnosis based on database, 2013 IEEE International Conference on Bioinformatics and Biomedicine, Shanghai, China, pp. 61-66. https://doi.org/10.1109/BIBM.2013.6732639
-
Kim JC, Chung K, (2020): Neural-network based adaptive context prediction model for ambient intelligence. J Ambient Intell Human Comput 11, 1451–1458. https://doi.org/10.1007/s12652-018-0972-3
-
Kim JC, Chung K, (2020): Neural-network based adaptive context prediction model for ambient intelligence. J Ambient Intell Human Comput 11, 1451–1458. https://doi.org/10.1007/s12652-018-0972-3
-
Jianfang W, Ruo H, Ming L, Shanshan L, Xizheng Z, Jun H, Jiaxu C, Xiangjun L (2021): Diagnosis of sleep disorders in traditional Chinese medicine based on adaptive neuro-fuzzy inference system, Biomedical Signal Processing and Control, Volume 70. https://doi.org/10.1016/j.bspc.2021.102942
-
Humenberger M (2010): Medizintechnische Objektivierung der chinesischen Pulsdiagnostik, Dissertation, Graz. https://online.medunigraz.at/mug_online/wbAbs.getDocument?pThesisNr=19901&pAutorNr=&pOrgNr= accessed on March 7th, 2023.
-
Lan KC, Litscher G, Hung TH (2020): Traditional Chinese Medicine Pulse Diagnosis on a Smartphone Using Skin Impedance at Acupoints: A Feasibility Study. Sensors. 2020; 20(16):4618. https://doi.org/10.3390/s20164618
-
Yan Tang AC (2012): Review of Traditional Chinese Medicine Pulse Diagnosis Quantification. Complementary Therapies for the Contemporary Healthcare. https://doi.org/10.5772/50442
-
Chaoxun G, Zhixing J, Haoze H, Yining L, David Z (2022): Wrist pulse signal acquisition and analysis for disease diagnosis: A review, Computers in Biology and Medicine, Volume 143. https://doi.org/10.1016/j.compbiomed.2022.105312
-
Wang X, Liu J, Wu C, Liu J, Li Q, Chen Y, Wang X, Chen X, Pang X, Chang B, Lin J, Zhao S, Li Z, Deng Q, Lu Y, Zhao D, Chen J (2020): Artificial intelligence in tongue diagnosis: Using deep convolutional neural network for recognizing unhealthy tongue with tooth-mark. Comput Struct Biotechnol J. 2020 Apr 8;18:973-980. https://doi.org/10.1016/j.csbj.2020.04.002
-
Xu Q (2020): Multi-Task Joint Learning Model for Segmenting and Classifying Tongue Images Using a Deep Neural Network, in IEEE Journal of Biomedical and Health Informatics, vol. 24, no. 9, pp. 2481-2489. https://doi.org/10.1109/JBHI.2020.2986376
-
Yang Z, Zhao Y, Yu J, Mao X, Xu H, Huang L (2022): An Intelligent Tongue Diagnosis System via Deep Learning on the Android Platform. Diagnostics; 12(10):2451. https://doi.org/10.3390/diagnostics12102451
-
Matos LC, Machado JP, Monteiro FJ, Greten HJ. Can Traditional Chinese Medicine Diagnosis Be Parameterized and Standardized? A Narrative Review. Healthcare. 2021; 9(2):177. https://doi.org/10.3390/healthcare9020177
-
Song J, Yang L, Su S, Piao MY, Li BL, Yu Y, Yu WY, Zhang M, Liang LX, Zuo GW, Tang ZM, Long YQ, Chen XL, Dai N, Mo JL, Wang RQ, Chen J, Hou XH (2020): Agreement of gastroenterologists in traditional Chinese medical differential diagnosis of functional dyspepsia compared with traditional Chinese medical practitioners: A prospective, multicenter study. J Dig Dis. Jul;21(7):399-405. https://doi.org/10.1111/1751-2980.12873
-
Ho LT, Chung VC, Wong CH, Wu IX, Lan KC, Wu D, Yeung JW, Zhang NL, Leung TH, Wu JC (2021): Evaluating traditional Chinese medicine diagnostic instruments for functional dyspepsia: systematic review on measurement properties. Integr Med Res. 2021 Sep;10(3):100713. https://doi.org/10.1016/j.imr.2020.100713